Fixed cutaneous sporotrichosis
Published Web Location
https://doi.org/10.5070/D330m45342Main Content
Fixed cutaneous sporotrichosis
Matthew J Mahlberg MD, Rishi Patel MD, Karla Rosenman, Wang Cheung MD, Nadia Wang MD, Miguel Sanchez MD
Dermatology Online Journal 15 (8): 5
Department of Dermatology, New York UniversityAbstract
Sporotrichosis is a subcutaneous mycosis that is caused by Sporothrix schenckii. Whereas the most common clinical presentation is the lymphocutaneous form, the fixed cutaneous form is not uncommon. Important clues from the clinical history, such as travel and occupation, can help to raise the suspicion of this infection in the differential diagnosis. However, histopathologic and tissue culture, which often require multiple specimens, are necessary to confirm the diagnosis. We present a patient with fixed cutaneous sporotrichosis whose delayed diagnosis led to appreciable scars and morbidity.
 |  |
| Figure 1 | Figure 2 |
|---|
History
A 21-year-old man initially presented to the Dermatology Clinic at Bellevue Hospital Center in June, 2008, with a 15-month history of enlarging skin lesions on the posterior aspect of the neck, shoulders, and back. These lesions had begun while he was living in Mexico and had persisted after he moved to the United States. He had been evaluated at another dermatology clinic where biopsies and cultures were performed. A definitive diagnosis was not made. Empiric treatment had been attempted with oral terbinafine and topical ketoconazole and with liquid nitrogen and curettage without benefit. These areas were not painful and not pruritic. There was no fever, chills, sweats, or weight loss. No pulmonary or neurologic symptoms were identified. The patient did not have a history of human immunodeficiency virus infection or other forms of immunosuppression and was taking no medications. He currently works as a waiter in a restaurant but had previously worked in agriculture.
Physical Examination
There were extensive, hyperpigmented, erythematous plaques with overlying verrucous, hyperkeratosis on the posterior aspect of the neck and on the posterior portion of the shoulders. No clavicular, postauricular, axillary, infraclavicular, or supraclavicular lymphadenopathy was noted.
Laboratory data
A comprehensive metabolic profile and complete blood count were normal. Bacterial culture demonstrated methicillin-sensitive Staphylococcus aureus. Mycobacterial culture demonstrated no growth. Fungal culture demonstrated Sporothrix schenckii.
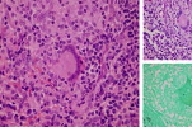
Histopathology
There is pseudoepitheliomatous hyperplasia and diffuse granulomatous and lymphoplasmacytic inflammation with dermal fibrosis. A periodic acid-schiff and Gomori methenamine silver stains demonstrate scattered single 9 to 10 micro, round fungal spores within the dermis in or around giant cells without evidence of capsule, pseudocapsule, or budding.
Comment
Sporotrichosis is the most common of the deep mycoses, which clinically presents with subacute or chronic cutaneous nodules and plaques and more rarely as systemic disease. The condition is caused by the direct traumatic inoculation of Sporothrix schenckii into the skin or by respiratory inhalation of spores. It was first described in 1898 at Johns Hopkins by a medical student named Benjamin Schenk, who cultured the organism from a 36-year-old patient, who had developed ascending nodules on the arm that appeared after a puncture wound [1].
The causative organism, Sporothrix schenckii, is a dimorphic fungus that is ubiquitously found in the environment. It can be cultured from grain, soil, wood, marine animals, and some insects. Gardeners, florists, and agricultural workers are at increased risk due to more frequent exposure to the fungus. Zoonotic spread from cats and armadillos also has been reported [2, 3]. Sporotrichosis is endemic in Mexico, Central and South America, and some areas of South Africa, which perhaps represents increased fungal prevalence or increased risk factors [4]. A recent epidemic of sporotrichosis related to cats has been identified in Brazil [5, 6].
The clinical presentation of sporotrichosis varies by site of inoculation, size of inoculation, and the immune status of the host [7]. The most common form of sporotrichosis is the lymphocutaneous form, which accounts for 75 percent of all cases. In this pathognomonic form, a papule or nodule may arise at the site of initial inoculation, which often is the hand, with development of additional lesions more proximally along the path of lymphatic drainage. A less common form, fixed cutaneous sporotrichosis, presents as a localized nodule or plaque, often with a granulomatous or verrucous appearance. This form most commonly occurs on the face, neck, trunk, or legs. Disseminated and extracutaneous disease rarely arises from hematogenous spread of initial inoculation from a respiratory or cutaneous source. In this form, the lungs, meninges, joints, and skin may become involved. Disseminated and extracutaneous disease is almost invariably associated with an immunocompromised state [8].
Diagnosis of clinical presentations different than the commonly-associated sporotrichoid pattern may be difficult or delayed because there may be resemblance to other conditions, such as atypical mycobacteria, nocardia, and other deep fungal infections. Fungal forms, when present, may appear as oval-to- cigar-shaped yeast; however, they are rare on histopathologic examination, so tissue culture is the gold standard for diagnosis. Other diagnostic methods include polymerase chain reaction and serologic tests, which are not readily available [9, 10].
A recently modified treatment regimen was unveiled by an expert panel of the Infectious Diseases Society of America in 2007 [11]. For primary lymphocutaneous and fixed cutaneous forms of disease, itraconazole therapy for three to six months is the first-line choice, followed by alternative antifungal agents or longer courses of itraconazole if treatment is unsuccessful. Disseminated and extracutaneous forms are treated more aggressively, with amphotericin B as a first-line agent.
References
1. Schenck BR. On refractory subcutaneous abscesses caused by a fungus possibly related to the sporotricha. Johns Hopkins Hosp Bull 1898; 9: 2862. Wenker CJ, et al. Sporotrichosis in a nine-banded armadillo (Dasypus novemcinctus). J Zoo Wildl Med 1998; 29: 478 [PubMed]
3. Xavier MH, et al. Cat-transmitted cutaneous lymphatic sporothricosis. Dermatol Online J 2008; 14: 4 [PubMed]
4. Sobera JO, Elewski BE. Fungal diseases. In: Bolognia JL, et al. eds. Dermatology, 2nd ed. London: Mosby, 2008: 1152
5. Hay RJ, Morris-Jones R. Outbreaks of sporotrichosis. Curr Opin Infect Dis 2008; 21: 119 [PubMed]
6. Schubach AO, et al. Epidemic cat-transmitted sporotrichosis. N Engl J Med 2005; 353: 1185 [PubMed]
7. Ramos-e-Silva M. Sporotrichosis. Clin Derm 2007; 25: 181 [PubMed]
8. Stalkup JR, et al. Disseminated cutaneous sporotrichosis treated with itraconazole. Cutis 2002; 69: 371 [PubMed]
9. Sra KK, et al. Molecular diagnosis of infectious diseases in dermatology. J Am Acad Dermatol 2005; 53: 749 [PubMed]
10. Hu S, et al. Detection of Sporothrix schenckii in clinical samples by a nested PCR assay. J Clin Microbiol 2003; 41: 1414 [PubMed]
11. Kauffman CA, et al. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis 2007; 45: 1255 [PubMed]
© 2009 Dermatology Online Journal

